Bloodstream Infections by Extended-spectrum β-lactamase-producing Klebsiella Species in Children
Extended-spectrum β-lactamase-producing Klebsiella Infections
DOI:
https://doi.org/10.4274/jpea.2023.238Keywords:
Extended spectrum β-lactamase, Klebsiella pneumoniae, Klebsiella oxytoca, childrenAbstract
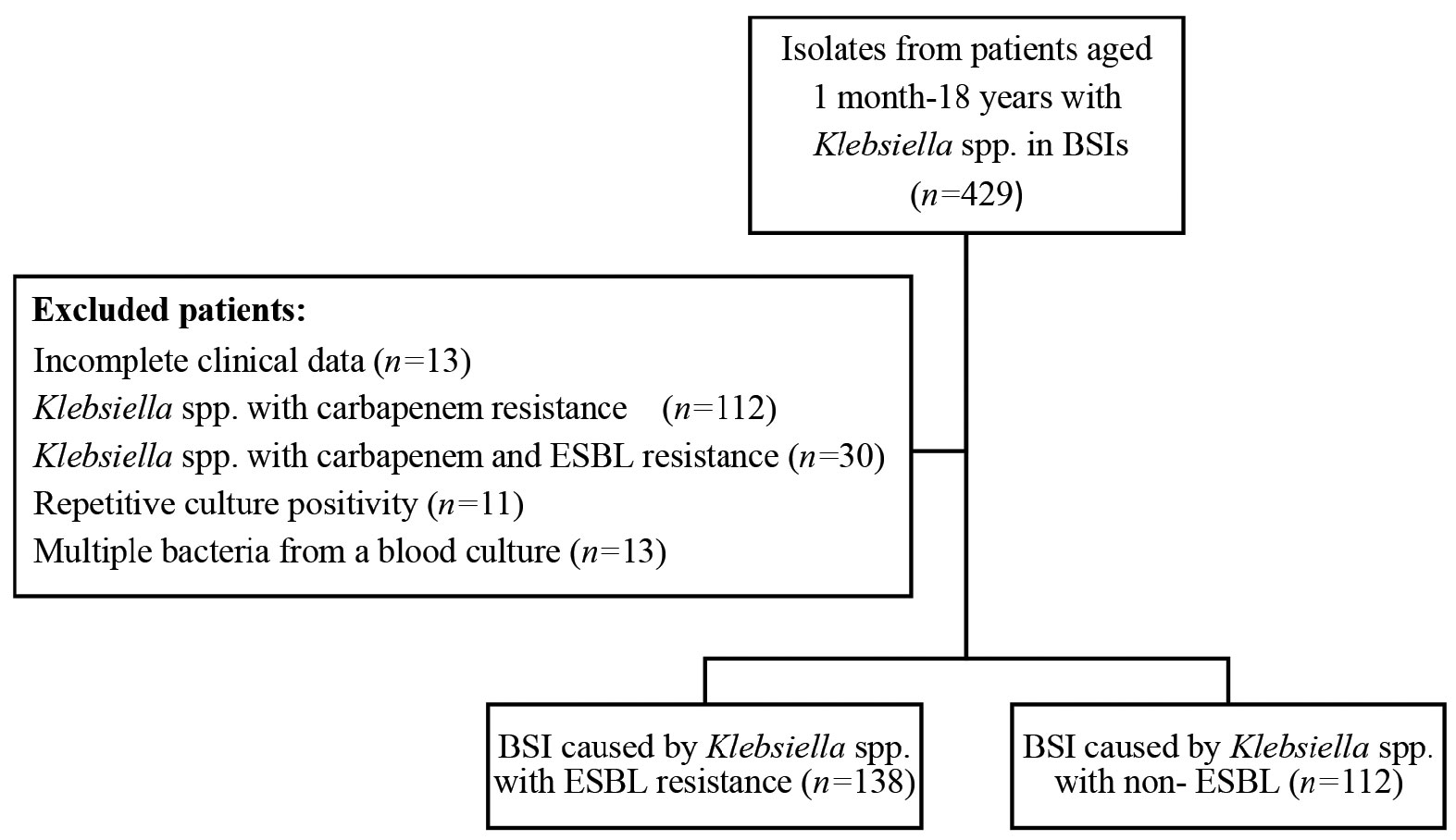
Infections caused by resistant Gram-negative bacteria are a serious public health problem, with Klebsiella spp. being the most common cause and increasing over the years. There is a striking increase in antibiotic resistance worldwide. The aim of this study was to retrospectively evaluate the characteristics and treatment of bloodstream infections (BSIs) caused by Klebsiella spp. and to identify possible risk factors for extended-spectrum β-lactamase (ESBL) resistance in our hospital between August 2019 and March 2023. Of 250 Klebsiella isolates, 112 (44.8%) were ESBL producers and 138 (55.2%) were ESBL nonproducers. Catheter-related BSIs (CRBSIs) accounted for 49.6% of infections and were more common in the ESBL nonproducer group. Most of the Klebsiella spp. were K. pneumoniae (233/250). Most of the infections were healthcare-associated infections (85.6%). Most patients had an underlying disease, the most common underlying disease in the ESBL-producing group was neurometabolic disease (26.8%), whereas in the ESBL-non-producing group it was malignancy (35.5%). The median age of the ESBL-producing group was 14 months and was younger (p=0.01). Previous antibiotic use in the last 30 days, especially aminoglycosides (p<0.006), β-lactam-β-lactamase inhibitor combinations (p<0.001) and cephalosporins (p<0.001), increased ESBL-resistant infection. Use of β-lactam-β-lactamase inhibitor combinations in the last 30 days increased the risk of ESBL resistance by approximately 7.4 times, and cephalosporins increased the risk by 5 times. In the ESBL-producing group, the median duration of treatment was longer at 14 days (p=0.01), and carbapenems were most commonly used (p<0.001). Thrombocytopenia (p=0.003), elevated C-reactive protein (p<0.001), CRBSI (p=0.009), presence of central venous catheter (p=0.03), urinary catheter (p<0.001), mechanical ventilation (p<0.001), intensive care admission (p=0.005), previous use of carbapenems, aminoglycosides, fluoroquinolones in the last 30 days (p=0.003, p=0.001, p=0.006, respectively) and colistin treatment (p<0.001) increased the risk of mortality. The 28-day mortality rate was 11.6%. Appropriate use of narrow-spectrum antibiotics and reduction of invasive procedures is important in reducing ESBL resistance and BSI-related mortality.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Journal of Pediatric Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.