Analyse of Febrile Neutropenia Attacks in Children with Acute Lymphoblastic Leukemia
Febrile Neutropenia with Acute Lymphoblastic Leukemia
DOI:
https://doi.org/10.4274/jpea.2023.225Keywords:
Acute lymphoblastic leukemia, children, febrile neutropeniaAbstract
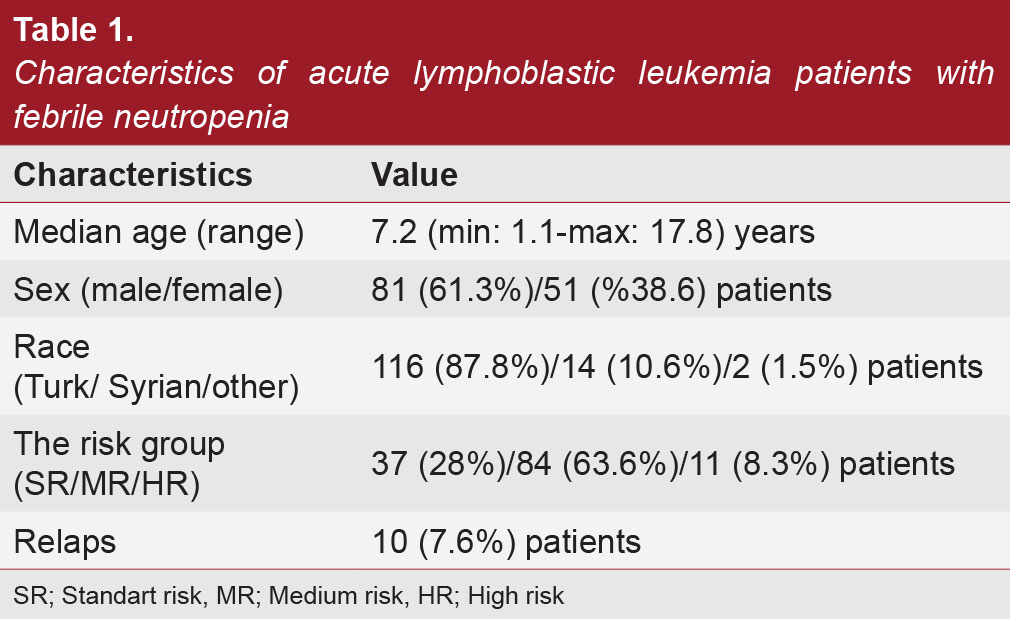
Febrile neutropenia (FN) is the most important cause of morbidity and mortality during treatment in childhood with acute lymphoblastic leukemia (ALL). The aim of this retrospective study was to assess clinical features, outcomes, treatment modalities, documented infection rates, and frequency of isolation of specific organisms from ALL patients treated by our Department of Pediatric Hematology and Oncology using Berlin-Frankfurt-Munich (BFM) protocols. In this study 132 children diagnosed with ALL and treated according to the ALL-BFM 2009 protocol at Kayseri City Hospital, Department of Pediatric Hematology and Oncology between July 2015 and May 2022 were enrolled and evaluated for episodes of FN during intensive chemotherapy. Treatment characteristics, the presence of relapse, duration of neutropenia, culture results, the choice and duration of antibiotics, and disease prognosis were retrospectively assessed using patient records. In 132 acute leukemia cases, 278 episodes of FN were observed aged 1.1 and 17.8 years (mean 7.1±4.9 years) in a male to female ratio of 1.5:1. Infection focus could be documented in 66 episodes (23.7%); pulmonary infections in 23 patients (34.8%), gastrointestinal tract infections in 20 patients (30.3%), in 10 patients urinary tract infections (15.1%), derma¬otological and soft tissue infections in 2 patients (3%). The causative infectious agent could be demonstrated in 92 (33%) episodes. The most common site of isolation was blood (86/92, 30.9%). While the most frequently identified bacterial infectious agents were Gram-positive bacteria (56 isolates, 20.1%), Gram-negative bacteria were identified in 28 isolates (n=10%). Fungal growth was detected in 6 (2.1%) patients and polymicrobial growth was detected in 3 (1.1%) patients. Of the 132 patients, 4 (3%) died due to infection 2 died during induction, and 2 died during reinduction phases. Centers should evaluate their results to identify changing epidemiological patterns and to treat FN early and efficiently.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Journal of Pediatric Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.